Continuous Positive Airway Pressure (CPAP) therapy is the leading treatment for obstructive sleep apnea (OSA), a condition where breathing repeatedly stops and starts during sleep. A CPAP machine provides restorative rest by delivering a constant stream of air to keep your airway open.
The specific pressure required is carefully calibrated to your unique anatomy. However, major life events like pregnancy, menopause, and significant weight changes can introduce hormonal changes that alter your body and breathing patterns, leading to emotional symptoms and physical changes.
Even a small physical shift can introduce new challenges to your CPAP treatment, such as mask leaks or the need for a new therapeutic pressure. Understanding how to adapt your CPAP therapy during these transitions is key to maintaining its effectiveness and ensuring good sleep quality.
Recognizing the early signs that your therapy needs an adjustment will help keep your treatment on track, improve your sleep quality, and keep your energy levels high. Here's everything you need to know about maintaining effective treatment during these important life changes
CPAP Use for Pregnant Women During Pregnancy
Pregnancy is a time of profound physiological and hormonal changes that affect a woman's body throughout every gestational age of her pregnancy. The pregnancy hormones, like progesterone, increase blood volume and fluid retention, which often leads to nasal congestion and soft-tissue swelling in the pharynx.
Hormonal changes and significant weight gain during pregnancy can raise a woman's risk for sleep apnea or make existing sleep apnea worse. Proper management during pregnancy is key.
Staying vigilant with consistent CPAP use is crucial for ensuring maternal and fetal well-being throughout the pregnancy. According to studies, the prevalence of obstructive sleep apnea (OSA) is higher in pregnancies affected by obesity and significant weight gain.
Untreated sleep apnea during pregnancy is linked to complications like gestational diabetes, cardiovascular diseases, gestational hypertension, preeclampsia, preterm birth, and even preterm delivery, making consistent CPAP therapy essential for pregnant women.
Pregnancy can increase the risk of gestational diabetes and require lifestyle changes. Women with gestational hypertension need careful monitoring for signs of vaginal bleeding and other pregnancy complications. These are serious risks for both the mother and baby during pregnancy.
Monitoring & Adjusting CPAP Use During Pregnancy
If you are pregnant, it is critical to monitor your CPAP therapy, since your pressure needs may change. Nevertheless, to repeat your sleep study is typically considered only if symptoms of sleep‑disordered breathing return or significantly worsen, such as:
- Loud snoring
- Witnessed apneas
- Excessive daytime sleepiness
- Worsening hypertension or gestational diabetes (which can be associated with OSA)
It's important to mention that to repeat a sleep test is a clinical judgment call, not a routine guideline, therefore the decision must be taken by your physician.
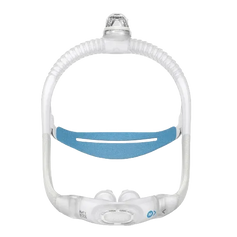
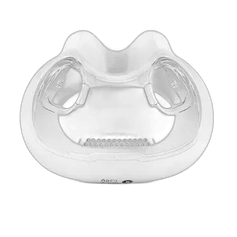
These changes during pregnancy can also affect how your CPAP mask fits. Facial swelling from the pregnancy may cause leaks, requiring a new cushion size or a switch to a less invasive option like a Wisp Nasal CPAP mask.
Heated humidification can soothe nasal passages affected by the hormones of pregnancy, and CPAP pillows with special cut-outs can help pregnant women find a comfortable sleeping position.
|
Key Insight: Your Auto-CPAP machine’s data is invaluable during pregnancy. Regularly review nightly reports with your doctor to proactively identify trends and adjust therapy before symptoms return. |
Navigating Menopause Symptoms and Hot Flashes with CPAP Therapy
The menopause symptoms and hormonal shifts impact sleep-disordered breathing. This transition, which can occur as premature menopause, is defined by changes in the menstrual cycle and the end of menstrual periods. The North American Menopause Society confirms that risk factors change significantly after menopause.
The hormones involved in menopause cause many changes throughout the body. As key hormones like estrogen and progesterone levels decline during menopause, upper-airway muscles can lose tone, making the pharynx more susceptible to collapse during sleep.
This is a common effect of menopause. The cessation of the menstrual cycle is a hallmark of menopause. Research confirms that while women may have a lower risk for obstructive sleep apnea than men in early life, this changes significantly after menopause.
The hormonal changes of menopause lead to common menopause symptoms like frequent hot flashes and night sweats. These hot flashes are a classic sign of menopause. Experiencing these flashes can create new comfort challenges with CPAP therapy during menopause.
Wearing a mask during the hot flashes of menopause can feel warm and restrictive. Fortunately, many modern ResMed CPAP mask options are designed with breathable, lightweight headgear to improve comfort during these menopause-related hot flashes. Managing CPAP during menopause is achievable.
Choosing a mask with minimal contact, such as the P30i mask, can help reduce feelings of claustrophobia. The discomfort from menopause symptoms, which can range from hot flashes and mood changes to vaginal dryness, makes comfortable CPAP treatment essential during menopause.
You can add moisture-wicking mask liners to absorb perspiration from hot flashes. The menopause transition, marked by irregular menstrual periods, signals the onset of these changes leading to full menopause. Many women explore hormone therapy to manage their menopause symptoms.
Adjusting your humidifier settings can also make a significant difference. The North American Menopause Society provides extensive resources on managing the various menopause symptoms and understanding hormone therapy.
|
Key Insight: The hormonal shifts of menopause are a major trigger for sleep apnea. The prevalence of OSA during menopause can increase post-menopause. |
The Impact of Gaining or Losing Weight
Body Mass Index (BMI) has a direct correlation with OSA severity, as excess weight gain and fatty tissue in the neck can narrow the airway. Starting a successful weight loss journey through increased physical activity and consuming fewer calories can significantly lessen airway obstruction.
This improvement often leads to a need for lower CPAP pressures as breathing becomes easier. Conversely, gaining weight, a common contributor to obesity, can increase airway collapsibility and require a higher pressure setting on a device like the AirSense 11.
This weight gain often necessitates a change in CPAP pressure settings. A substantial change in your total weight is one of the most common reasons for a CPAP pressure retitration.
Your doctor will likely recommend a new sleep study after bariatric surgery or if you gain weight significantly, which can exacerbate obesity. These changes also alter your facial contours, which means a mask that once fit perfectly may now leak.
It is important to re-measure and adjust your headgear regularly to account for changes in your weight and metabolism. As you navigate through major life changes, consider these important risk factors and prevention strategies for maintaining effective CPAP treatment:
| Life Change | Associated Risks | Prevention Measures |
| Pregnancy | Preeclampsia | Consistent CPAP use |
| Menopause | Increased OSA risk | Proper Mask Selection |
| Weight Changes | Mask leaks | Regular Assessment |
|
Pro Tip:Don't wait for symptoms to return after significant weight changes. Proactively schedule a CPAP re-titration discussion with your doctor after losing or gaining weight to ensure your pressure settings remain optimal and effective, especially after weight gain. |
Working With Your Care Team
You are not alone in navigating these changes. Your optimal support circle includes healthcare professionals dedicated to your respiratory health and sleep quality.
This team also includes your sleep physician, who diagnoses sleep disorders, and your reliable Durable Medical Equipment (DME) provider, like RespShop, who supplies machines and ResMed CPAP supplies for your treatment.
A Registered Respiratory Therapist (RRT) is a clinical expert who can help fine-tune equipment settings and troubleshoot mask fit issues. You can use remote monitoring or your machine's SD card to share data with your care team.
This allows them to spot trends early and make adjustments proactively before issues arise with your continuous positive airway pressure therapy or equipment, including specialized devices like VPAP machines.
|
Key Insight: You are the most important member of your care team. Proactively sharing your machine's data with your sleep physician and RRT allows them to spot trends and make adjustments before problems arise. |
How We Support You Through Life Changes
At RespShop, we understand that your CPAP therapy needs evolve, and we provide the tools and expertise to support you at every stage of these lifestyle changes. Our team of certified sleep science coaches offers complimentary consultations on equipment, mask fitting, and therapy optimization.
We aim to provide a wide range of sleep solutions to meet your changing needs. Whether you need a new primary device, a lightweight travel machine, or a temporary solution through our CPAP rental program, we have flexible options.
We offer a variety of equipment to fit every budget and ensure you receive the best value for your health investment, and improve your overall sleep quality.
Maintain Effective CPAP Treatment
Life is a dynamic journey, and your continuous positive airway pressure (CPAP) therapy should adapt with you. Pregnancy, menopause, and substantial weight changes like weight gain can all impact your airway anatomy and pressure requirements.
By staying proactive, you can ensure your CPAP treatment remains effective, and your sleep remains restorative.
Track your therapy data, be mindful of emerging symptoms, and never hesitate to work with your care team to recalibrate your pressure or swap your mask for a better fit.
Have questions about adjusting your CPAP setup? Our registered respiratory therapists are here to help. Contact Us to get personalized advice.